Charge Capture
A digital superbill is generated based on documentation on the EHR. Once the note is signed off, the suggested codes will be available on the PM where our dedicated team of billers will review to achieve clean claim submission.
Claim Submission and Management
Our team, comprised of dermatology billing experts, will review and submit claims electronically to the clearinghouse or via paper when needed. We will handle each claim from start to finish, including first & secondary filings and follow-up on unpaid claims.
Rejection & Denial Management
We manage claim denials, rejections, and exclusions. Our dedicated team works diligently making sure no claim is left behind. We document all our notes within the system for full transparency.
Payment Posting
Our billing experts process, match, and post payments (electronic and paper) to maintain accurate records of how insurance and patient payments are allocated.
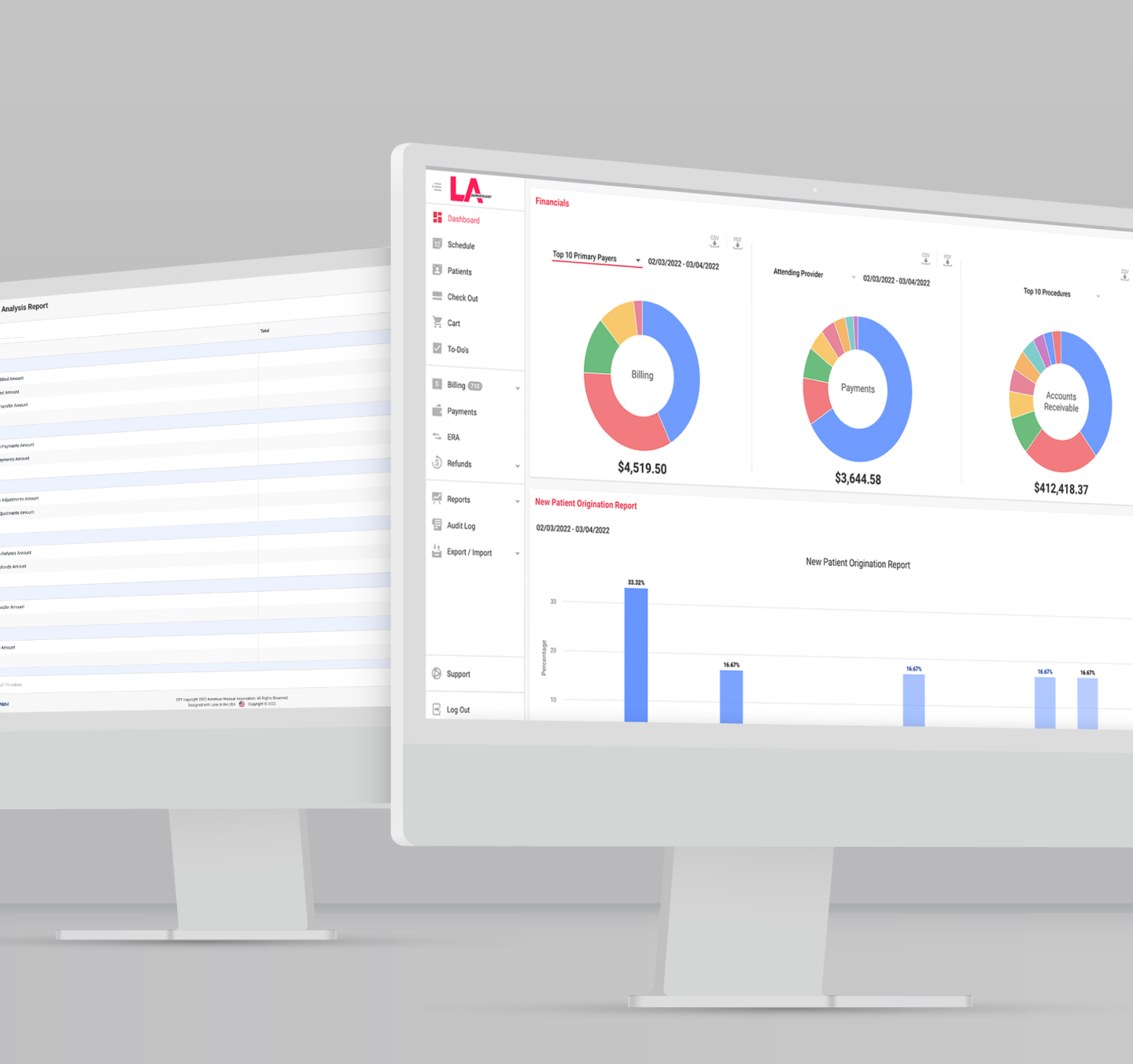
A/R Follow-Up and Analytics
A/R policies and procedures are in place to collect on any outstanding claims. With our real-time aging report and other analytics, you’re able to monitor your financial performance as our team works to get you paid.
Patient Statements, Collections and Inbound Call Center
Patient statements are managed by our team to stay on top of patient aging and assisting in patients being sent to collections if needed. We also provide phone support to your patients if they have any questions about their bill, plan benefits, and out-of-pocket costs.